- (512) 368-3238
- info@houseofrcm.com
- Taxes, USA
- 5900 BALCONES DRIVE STE 100 AUSTIN TX 78731
Solutions for your success
Our Products and Services
Telehealth Services
Telemedicine is now vital, driven by technology and the demand for remote care, especially post-COVID-19. House of RCM LLC has the expertise to navigate the unique billing challenges of telehealth. We support providers of all sizes, from individual physicians to large medical groups, with tailored solutions for revenue cycle management and telehealth service development.


Medical Billing Services
House of RCM LLC submits claims to all commercial insurers, including Medicare, Medicaid, and Workers’ Compensation. We file claims with primary and secondary insurers and ensure accurate payment processing for maximum reimbursement. Patient statements are sent for co-pays, co-insurance, or deductibles, and our customer support team is readily available to address any billing questions or concerns. We prioritize transparency and clear communication with both healthcare providers and patients, ensuring that financial matters are managed smoothly and efficiently. Additionally, we offer customized reporting and analytics to help practices monitor their revenue cycle and make informed decisions for financial growth.
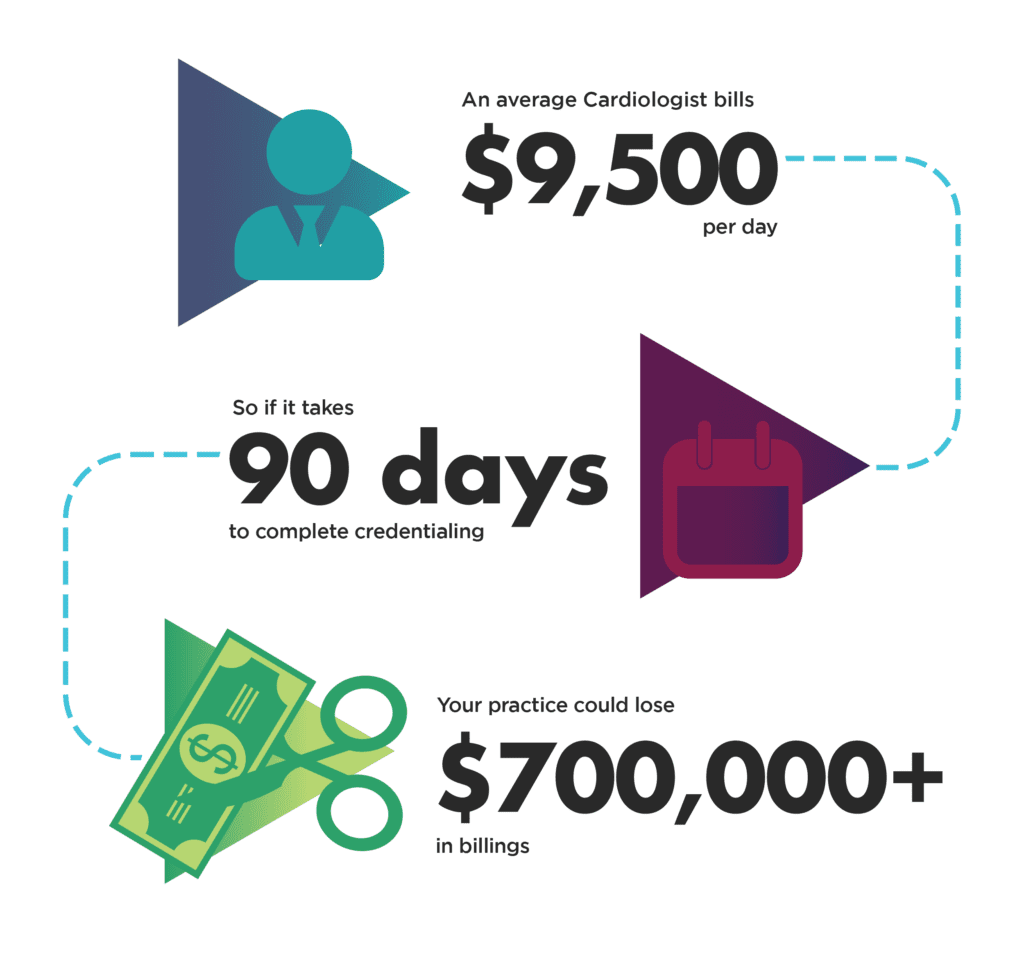
Credentialing and Enrollment
Medical credentialing can be complex, but at House of RCM LLC, we simplify the process. We ensure accurate enrollment with Medicare, Medicaid, and commercial payers, offering full enrollment, MAC configuration, and revalidation services. Whether you’re a solo practitioner or part of a multi-specialty team, we swiftly manage your credentialing needs. Our team handles all aspects of the credentialing process, including applications, re-enrollments, and updates, ensuring your credentials stay current to prevent payment delays. We also monitor deadlines and liaise with insurance companies to resolve issues, allowing you to focus on patient care while we manage the administrative tasks.

AR Services
Managing Accounts Receivable (AR) has become increasingly complex. The rise of various payment plans, co-insurance, and the growing number of patients with high-deductible health plans have made the payment landscape more intricate and uncertain. To navigate these challenges and improve cash flow, healthcare providers require a comprehensive strategy that effectively addresses these issues. At House of RCM LLC, we specialize in AR management, utilizing advanced technologies and proven methodologies to streamline the collection process and reduce outstanding balances. Our experts closely monitor unpaid claims, follow up diligently with both insurers and patients, and ensure that no revenue is lost due to delayed or missed payments. We provide detailed AR reports, allowing practices to track their receivables in real-time and make informed decisions on financial strategies. By addressing AR concerns proactively, we help reduce the strain on healthcare providers, enabling them to focus more on patient care rather than financial administration. We also offer flexible payment solutions for patients, making it easier for them to meet their financial responsibilities without delaying care.
Eligibility Verification and Prior Authorization
Prior authorization is a critical process that helps practices submit and recover approved claims, optimizing cash flow. Inefficient prior authorization can lead to increased denials and reduced revenue. Up to 65% of claims are denied due to ineligibility, making it a crucial yet underutilized step in the revenue cycle. At House of RCM LLC, we prioritize the prior authorization process to ensure smooth and efficient claim approvals. Our experienced team works closely with healthcare providers and insurers to verify patient eligibility and secure authorizations for services in advance, reducing the likelihood of claim denials. We maintain strict compliance with payer guidelines and ensure that all necessary documentation is submitted promptly to prevent delays in treatment and reimbursement. We also offer real-time tracking and follow-up on prior authorization requests, ensuring that any issues are addressed immediately to avoid treatment interruptions or revenue loss.


Payment Posting
Payment posting is a crucial part of the revenue cycle for any solo practitioner or healthcare organization. It involves posting payments, managing deposits, and ensuring reconciliation between posted payments and deposits. This process directly impacts other functions of the medical office, influencing patient satisfaction, operational efficiency, and overall financial performance. An efficient payment posting system offers real-time insights into a practice’s daily revenue stream, allowing for quick identification of potential issues and prompt corrections. It ensures your practice stays on top of insurance payments from EOBs, ERAs, patient payments, and more, giving you a clear, up-to-date financial snapshot.
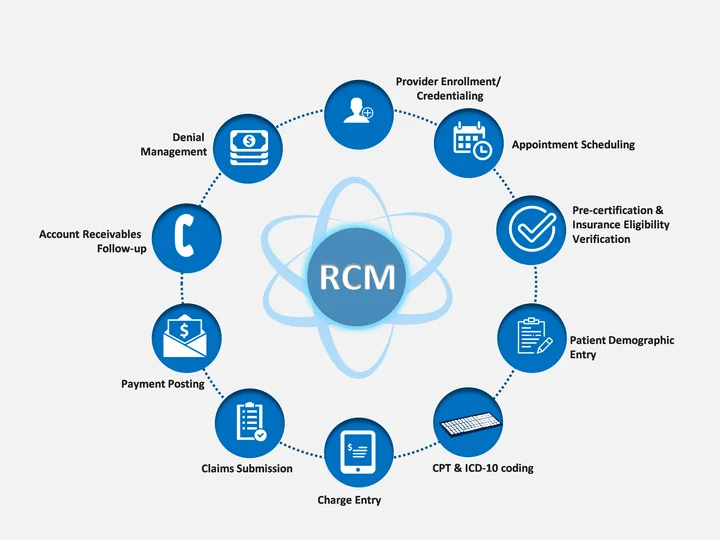
Complete RCM Service
All our RCM services are provided to you in a highly cost-effective and comprehensive manner. At the end of the day, our revenue cycle management services allow you to closely examine these critical financial figures, offering deeper insights into your revenue stream and enabling you to make informed decisions about your practice’s financial health and future planning.

Practice Management
At House of RCM LLC, we offer comprehensive practice management services meticulously designed to streamline the administrative and financial functions of healthcare providers. Our primary goal is to help practices operate more efficiently, improve patient satisfaction, reduce operational burdens, and maximize revenue potential for sustainable growth. Our practice management solutions cover everything from appointment scheduling and patient intake to billing, coding, and claims submission. We ensure that each step of the revenue cycle is optimized for accuracy and speed, reducing claim rejections and improving cash flow. Additionally, we implement efficient workflows and automated systems to minimize administrative overhead, allowing healthcare providers to focus more on patient care.
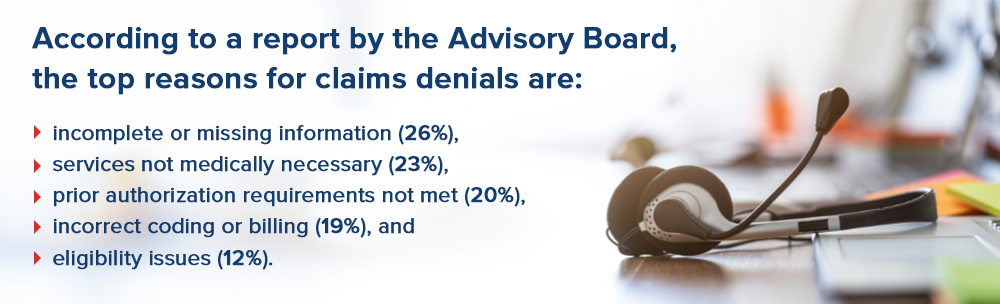
Denial Management
Denial management is a systematic approach to handling denied insurance claims in medical billing. It involves investigating each denial, conducting root cause analyses to understand why claims were denied, and identifying patterns or trends among insurance carriers. By redesigning or re-engineering processes, healthcare providers can prevent or reduce the risk of future denials. A denial occurs when a health insurance company refuses to pay for services or products it has agreed to cover.

Reporting
In today’s complex healthcare environment, evaluating medical billing performance has become increasingly intricate due to the expanded range of reporting options. To accurately assess specific practice performance processes that impact your revenue cycle—such as medical billing, patient pre-collections, and claim denial corrections—custom reports are essential. These tailored reports provide a unified source of data and metrics, enabling more effective assessment and comparison of billing and collection performance trends.
Customized Reporting
Medical billing reports can help you thoroughly understand the financial health of your practice. These detailed reports can provide insights into how your medical practice is performing across various revenue cycle metrics, identify whether claims are being paid on time, and reveal how efficiently insurance carriers are reimbursing your practice for critical procedures and services.

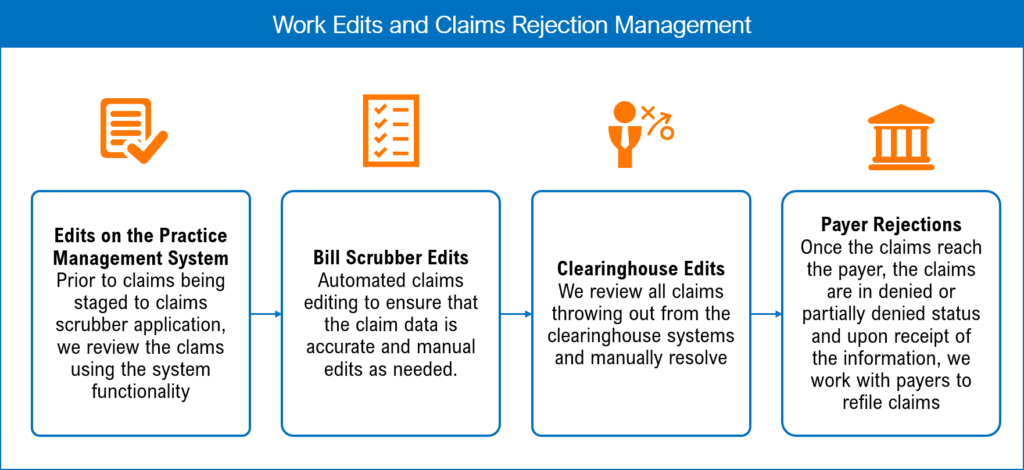
Claim Submission
The experienced team at House of RCM LLC is ready to assist you at every stage of the medical billing process. By outsourcing your medical claims submission services to us, you can lower overhead costs, boost revenue, and enhance the efficiency of your team. It determines the amount of reimbursement that the healthcare provider will receive after the insurance company clears the dues. We handle both primary and secondary claims, ensuring proper coordination of benefits and accurate billing. By monitoring the claims process closely, we promptly address any discrepancies or rejections, facilitating quick resubmissions to maintain a consistent revenue stream. Our streamlined claim submission process helps healthcare providers receive maximum reimbursement, improving overall cash flow.
Shopping Cart
There is no item in your cart
